For several years already, Myopain Seminars has offered canine dry needling courses in The Woodlands, TX and this year (2020) we plan to launch a completely new “Equine Dry Needling” course in Europe and the US. Developed by Maria Calatayud, PT, MSc, and Dr. Maria Resano, DVM, MSc, CERT, ESMT, CVA with the assistance of Jan Dommerholt, PT, DPT, the course is going to be a very practical hands-on course based on the current scientific evidence of dry needling.
Meet the instructors
 Ms. Maria Calatayud is a Spanish physical therapist. In 2008, she received her Master’s in Physiotherapy from the Cardenal Herrera CEU University in Valencia, Spain. She studied physiotherapy with the sole purpose of specializing in the physiotherapy treatment of horses. After graduation, she completed a Master’s in Osteopathic Manual Therapy while raising her children, followed by a Master’s in Equine Physiotherapy. She has completed advanced training in equine dry needling techniques in the Netherlands and equine Kinesio taping in the United Kingdom. To top it off, Maria also has a bachelor’s degree in Fine Arts, a Master’s in Graphic Design, and she is currently pursuing her Ph.D. focusing on equine myofascial pain and dry needling at the Universidad Autónoma of Barcelona.
Ms. Maria Calatayud is a Spanish physical therapist. In 2008, she received her Master’s in Physiotherapy from the Cardenal Herrera CEU University in Valencia, Spain. She studied physiotherapy with the sole purpose of specializing in the physiotherapy treatment of horses. After graduation, she completed a Master’s in Osteopathic Manual Therapy while raising her children, followed by a Master’s in Equine Physiotherapy. She has completed advanced training in equine dry needling techniques in the Netherlands and equine Kinesio taping in the United Kingdom. To top it off, Maria also has a bachelor’s degree in Fine Arts, a Master’s in Graphic Design, and she is currently pursuing her Ph.D. focusing on equine myofascial pain and dry needling at the Universidad Autónoma of Barcelona.

Dr. Maria Resano is a veterinary medicine physician. In 2003, she received her degree in Veterinary Medicine from the Faculty of Veterinary Medicine at the Universidad de Zaragoza in Spain. Following her veterinary studies, she completed an equine internship after which she decided to specialize in equine rehabilitation. She completed a Master’s degree in Equine Rehabilitation and Physical Therapy followed by externships in Kawell Equine Hospital (Argentina) and in the Rehabilitation Section of the Swiss Institute of Equine Medicine. She has multiple certifications in equine dry needling, equine Kinesio taping, equine sports massage, and veterinary acupuncture. Maria is a “Certified in Equine Rehabilitation Therapist” (CERT) by the Animal Rehab Institute in Florida, USA. She is currently pursuing her Ph.D. focusing on equine myofascial pain and dry needling at the Universidad Autónoma of Barcelona.
Together, they have presented at several conferences, such as
- “Improvement of myofascial pain in equine brachiocephalicus muscle using dry needling technique” – 9th International Symposium on Veterinary Rehabilitation and Physical Therapy IAVRPT, Sweden, 2016.
- “Intra-rater reliability in locating myofascial trigger points in the equine brachiocephalicus muscle” – 28 Jornadas de Fisioterapia . EUF ONCE-ETM TUPIMEK. “Fascia, avances científicos” – Madrid, 2018
- “Painful response to trigger point palpation in the equine brachiocephalicus muscle: a preliminary study” – 30 Jornadas de Fisioterapia. EUF ONCE-ETM TUPIMEK. “Sindroe de dolor miofascial y puntos gatillo miofasciales: 20 años de evolución, Madrid, 2018
In 2019, they published a study in Revista Fisioterapia Invasiva/Journal of Invasive Techniques in Physical Therapy:
Calatayud-Bonilla, M., Resano-Zuazu, M., & Segura-Ortí, E. (2019). Pain pressure thresholds for evaluating myofascial pain in the equine brachiocephalicus muscle. Revista Fisioterapia Invasiva/Journal of Invasive Techniques in Physical Therapy, 2(02), 114-114
Equine Myofascial Pain
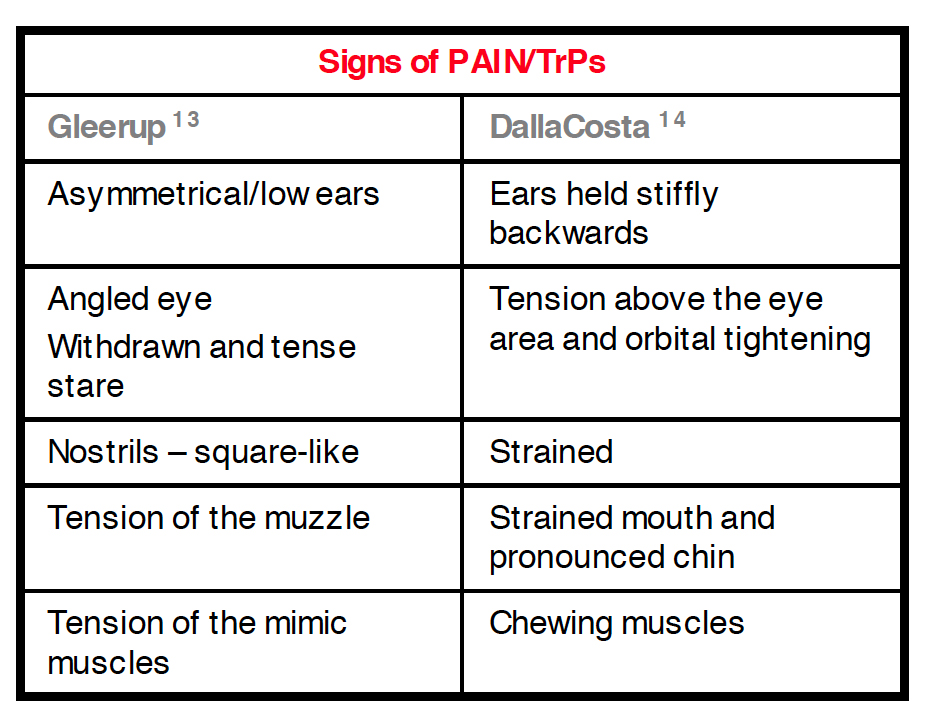
Identifying the source of pain in a horse can be challenging. A horse with an extremely sore back can have strong reactions even to very light palpation. The severity of the reaction is not always an indication of the severity of underlying disease; rather, it may simply be a result of inappropriate efferent discharge from facilitated interneurons, or what is commonly referred to as sensitization. Horses communicate their pain through their behavior.


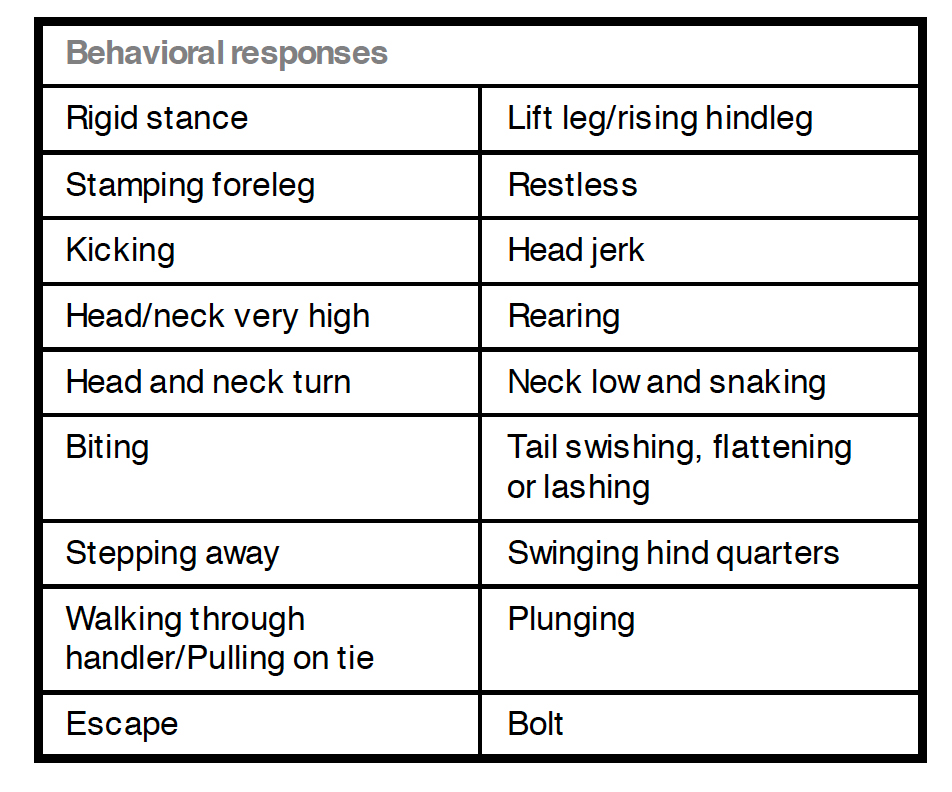
Several researchers have described the existence of trigger points (TrPs) in horses (von Schweinitz, 1999; Macgregor and von Schweinitz, 2006; Bowen et al. 2017), but equine dry needling is rarely mentioned in the scientific literature. Bowen and colleagues described the location of TrPs in the pectoral region of horses and recommended scoring the severity of TrPs based on the behavioral reaction to palpation. They associated these findings with girth-aversion behavior.
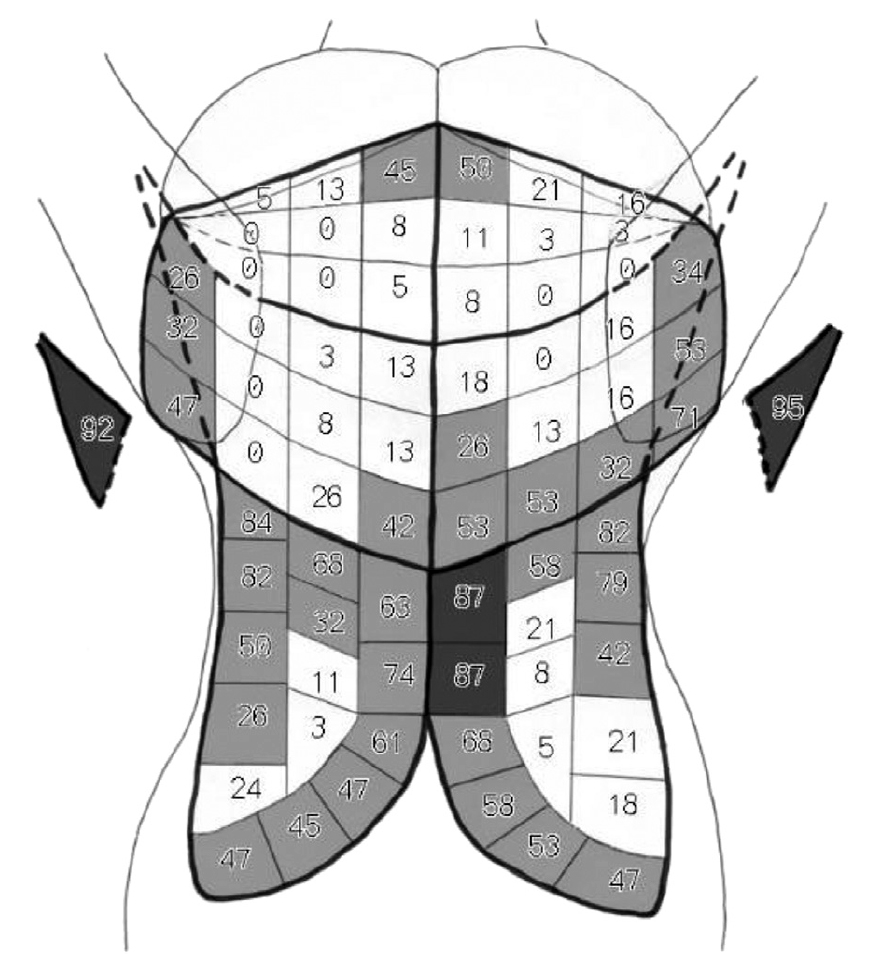
The authors palpated taut bands in 38 horses during a physiotherapy assessment. TrPs were scored as mild (6 horses), moderate (24 horses), and severe (8 horses). TrPs were identified in all horses with the axillary region as the most common region. Ninety-five percent of horses had TrPs in the right side ascending pectoral muscle and 92% on the left with a mean classification of severe covered by the girth. Eighty-seven percent of the horses presented with a mean classification of severe.
In this study, dressage and pony club horses had more TrPs than other disciplines, which was attributed to the variety of workloads, tack, and training methods used. Turning the head to look at the girth area while fastening the girth was the most common girth-aversion behavior seen in 50% of the horses. Horses with a history of girth–aversion behavior (n=13) had higher severity scores. Animals with girth-aversion behavior had more severe TrPs, which was a very important finding designing treatment strategies.
Macgregor and von Schweinitz explored for the first time the EMG characteristics of TrPs in the equine cleidobrachialis muscle, which is one of the two parts of the brachiocephalic muscle. Four horses showing signs of myofascial pain were recruited for treatments with acupuncture. All the horses demonstrated tender points in a taut band of muscle, which produced the same signs that are commonly found in humans (jump sign and local twitch responses or LTR on snapping palpation). If the location of the TrP corresponded to an acupuncture point appropriate for treatment, an examination with an EMG needle was performed at this point. A TrP at the acupuncture point LI16, located in the cleidobrachialis muscle, was the most frequently examined site for electromyographic activity. A total of 25 needle positions were examined at each TrP. Spontaneous electrical activity (SEA), spike activity and LTRs were recorded. If SEA was found, the TrP was considered active. Patients in this study showed signs of SEA, spike activity and LTR at the TrP sites compared to control sites and the type of electrical activity was similar to that found in human and rabbit skeletal muscle.
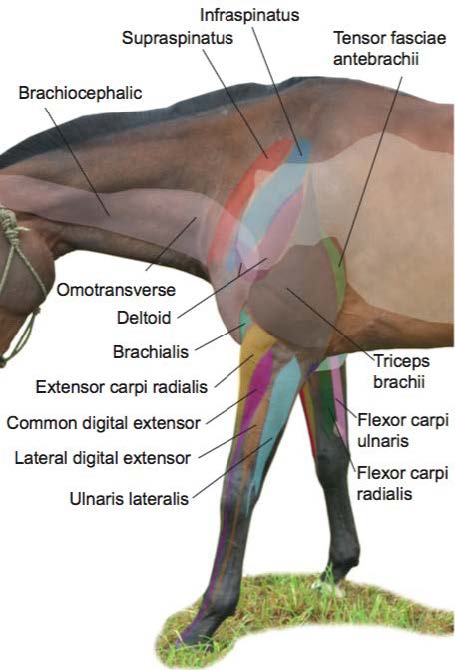
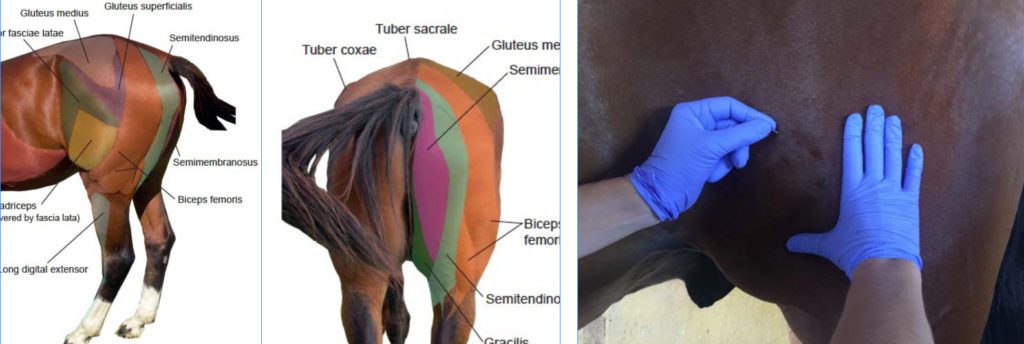
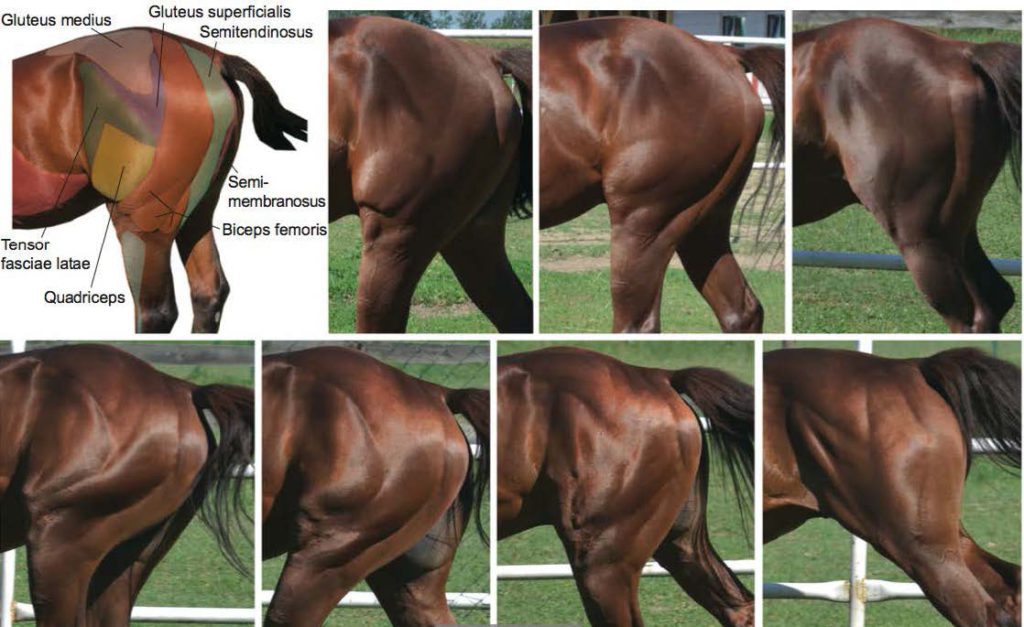
In horses, the most common muscles that develop TrPs in response to overuse or stress are the muscles of “ fright and flight,” which include muscles in the forehand such as the trapezius, brachiocephalicus, sternocephalicus, masseter, the infraspinatus muscles, paravertebral extensor muscles in the back area, the gluteal muscles, and the “hamstring” group of muscles. These muscle groups undergo shortening when in “fright and flight” posture (Ridgway 2005). The longissimus muscles, gluteals, biceps femoris, and semimembranosus and tendinosis muscles propel the horse and it is quite common to see dysfunctional movement patterns and even pathologic changes (Wolf 2002). Back problems are one of the most common musculoskeletal injuries in horses. Physical strain in the muscles of the back can be developed by improper shoeing, lack of appropriate dental work, poor equitation, poor saddle fit, overuse, improper training, and poor candidate selection (Ridgway 1999).
Equine Dry Needling

The indications for DN are similar for humans and horses, although there is little scientific evidence about equine DN. In equine DN, the same needles are used as used in human medicine. Some horses cannot be approached with a syringe or a needle. In those instances, oral detomidine (0.06 mg/kg) can be squirted into the mouth like a paste (Hubbell & Werner 2008). Preferable, the horse is treated outside the box tied with a quick-release knot and standing on a non-slippery surface. It is recommended to have rewarding treats for the horse. The treatment area should be quiet and free of noise and other distractions.

The clinician must wear comfortable clothing and safety shoes suitable for working with horses. At all times, clinicians must be aware of the horse’s reactions. The position of the clinician depends on which muscles are being treated. The assistance of a handler may be required in some cases.
Although there are protocols for hand hygiene and guidelines for skin antisepsis for equine surgery or other procedures such as central venous catheters, there are no formal published guidelines for acupuncture or DN hygiene.
The following are a few examples of equine dry needling. Clearly, without proper instruction, equine DN should not be performed!
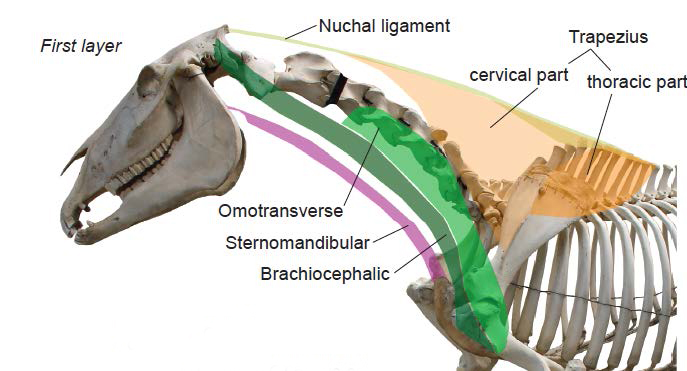
Brachiocephalic muscle
- Needling the brachiocephalic muscle will help the horse to performance lateral exercises with more suppleness
- It will help to release tension in lateroflexion of the neck
- It will also help the horse not to get engaged with the bit reducing the resistance on the riderʼs hand
- Facilitates flexion of the cervical spine
- Greater range of movement for protraction of the leg
Biceps Femoris muscle
The biceps femoris muscle is difficult to needle due to the thickness of the skin, but often it will relax after DN of the medial gluteal muscle. DN will improve rotation of the limb and the function of the three joints covered by the muscle: the hip, knee and tarsal joint.
As in human medicine, equine DN aims to reduce pain and facilitate optimal movement patterns. DN is not the ultimate goal of the therapy. It serves to facilitate better, pain-free movement and performance. As in canine DN, at this point, the effects of DN are mostly empirical. After several years of working with veterinarians and animal physical therapists in the canine DN courses, dry needling has made a tremendous difference for many patients. Our experiences with equine dry needling have been very positive. Equine DN is not completely new. There are a few other organizations that offer equine DN courses mostly in Europe. We recommend exploring all equine DN course programs in addition to the new Myopain Seminars Equine DN course. More information about course dates and locations will follow after the COVID-19 pandemic has passed on and we will be allowed to travel and gather again.

Register for Our Course
Myopain Seminars’ curriculum is developed by international leaders in dry needling and manual trigger point therapy. Our courses are a great way to bring a unique and innovative treatment option to your patients. Completing our course programs elevates your practice and expands your clinician’s toolbox to encompass a wide range of therapies that can effectively eliminate patient pain.
References
Gleerup, K. B., Forkman, B., Lindegaard, C., & Andersen, P. H. (2015). An equine pain face. Veterinary Anaesthesia and Analgesia, 42(1), 103-114
Dalla Costa, E., Minero, M., Lebelt, D., Stucke, D., Canali, E., & Leach, M. C. (2014). Development of the Horse Grimace Scale (HGS) as a pain assessment tool in horses undergoing routine castration. PLoS One, 9(3), e92281
Von Schweinitz, D. G. (1999). Thermographic diagnostics in equine back pain. Veterinary Clinics of North America: Equine Practice, 15(1), 161-177
Macgregor, J., & von Schweinitz, D. G. (2006). Needle electromyographic activity of myofascial trigger points and control sites in equine cleidobrachialis muscle–an observational study. Acupuncture in Medicine, 24(2), 61-70
Bowen, A. G., Goff, L. M., & McGowan, C. M. (2017). Investigation of myofascial trigger points in equine pectoral muscles and girth aversion behavior. Journal of Equine Veterinary Science, 48, 154-160
Ridgway, K. J. (2005). Diagnosis and treatment of equine musculoskeletal pain. The role of the complementary modalities: Acupuncture and Chiropractic. In Proceedings of the Annual Convention of the AAEP – Seattle, Washington, USA, 2005.
Ridgway, K. (1999). Acupuncture as a treatment modality for back problems. Veterinary Clinics of North America: Equine Practice, 15(1), 211-221
Wolf, L, (2002). The role of complementary techniques in managing musculoskeletal pain in performance horses. Veterinary Clinics of North America. Equine Practice, 18, 107-115, vii
Hubbell, J. A., & Werner, H. W. (2008, December). A review of the American College of Veterinary Anesthesiologists guidelines for anesthesia of horses. In AAEP Proceedings (Vol. 54, pp. 48-53).



