Louis Gifford’s Mature Organism Model is not just a very clever system to better understand pain mechanisms, but it can also be used as a therapeutic tool for patient education.
Gifford described a cycle of INPUT – SCRUTINIZING – OUTPUT that is able to facilitate itself, but that is also influenced by certain external factors, such as stress or other emotional situations. There is much data in support of the role of the human immune system on pain, peripheral and central processing of pain disorders and other, often complex diseases.
The Immune-System and Pain
The immune system consists of many organs and cells and is, next to the nervous system, the most complex organ system in the human body. It is working as a very effective protector against a multitude of pathogens like viruses, bacteria and other microorganisms. Furthermore, it monitors the body to effectively destroy tumor-like cells, that permanently grow in our body, and as such prevent cancer from developing. There are some immune reactions everybody knows quite well. These reactions are very important mechanisms to heal tissue damage or to survive diseases: -* Inflammation (distribution of histamine, leukotriene…) -* Fever (raising the bodies core-temperature to “kill” unfamiliar intruders) -* Building antibodies (e.g. influenza)
Neuro-Immunology
Our nervous system contains billions of neurons and nerve cells are connected to each other via billions of synapses. The structural and functional “neighbor” of these neurons are immune-cells, including microglia, astrocytes or oligodendrocytes. You have to imagine those “neighbor”-cells as silent observers. In contrast to neurons, those cells do not have the task or even the ability to send information from the periphery to the central nervous system and back (conduction). They are just interacting and communicating with the nervous system. As long as everything is okay, they remain quite silent, but as soon there is any intruder activation (viruses) or tissue-damage, they send their special tools to the specific location to start the healing processes via inflammation. They start to fight against bacterial infections via fever and macrophages, also called “eating-cells”.
We already know much about the function of the nervous system (peripheral nerves, the spinal cord and the brain) in acute and persistent pain mechanisms. Peripheral and central sensitization can develop and persist without tissue damage, because of sensitizing processes in the dorsal horn of the spinal cord. These processes work because of the release of neurotransmitters (e.g. glutamate or aspartate) that facilitate neuronal conduction to suprathalamic cortical areas. The brain determines whether the incoming stimulus is dangerous. Under certain circumstances the brain fails to differentiate accurately and normal touch or pain-free movements become painful due to this maladaptive processing.
What is the immune system’s role?
Though it is sometimes not very comfortable and annoying, we should be happy about the reactions of our immune system and the way it works. During the last fifteen years or so, scientists found that the immune system might also play an important role in the persistence of certain chronic pain disorders, especially microglia and astrocytes . It seems like those cells have an anti-inflammatory effect, as well as a pro-inflammatory effect, which may not sound very logical. Nevertheless, research in cell-physiology shows remarkable results. A prolonged or sustained nociceptive process can trigger microglia and astrocytes to start to releasing glutamate into the synaptic cleft, which means that the already sensitized dorsal horn gets even more sensitized and more “danger”-information has to be scrutinized in your brain.
A scenario you would not wish for…..
So maybe the following metaphor is not the best one, but it describes in simple words what is going on when your immune-system is influencing the nervous-system in its role of nociception:
“The alarm system (brain) of your beloved house and garden (body) is malfunctioning (maladaptive mechanism, central sensitization) so that it starts to yell and ring every time a cat (not dangerous) is entering the house via the backdoor. Neighbors (immune-cells), who watch your house most of the time, start to throw stones at your house and yell: “Hey, hey!!! Watch out, this cat it is dangerous, I remember this from the last time it entered your garden!!!”
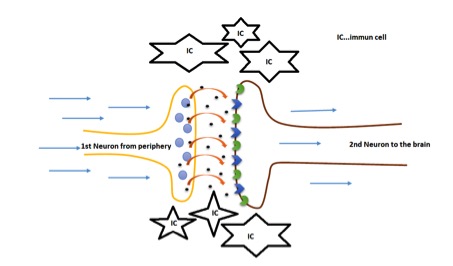
Simplified view into the dorsal horn: The immune cells start to facilitate sensitizing processes by pouring out neurotransmitters into the synaptic cleft!
Until now, the mechanisms of the neuro-immunological system are not completely understood, especially the role of the immune-cells, as a pro- and anti-inflammatory contributor remains unclear. What we know is, that the immune-system is under the control of our autonomic nervous system, which brings us to the importance of the psycho-immunological context of stress-disorders and pain.
Chronic headache is the second common persistent neuro-musculo-skeletal disorder right after persistent low back pain. Like all chronic pain disorders, it is important to consider this condition from a biopsychosocial perspective and to understand the patient within a holistic framework. It is important to carefully listen to your patients’ stories and to ask specific questions regarding health issues and yellow flags. With the knowledge of neuro-immunology, several chronic face and head syndromes can be viewed and managed in a different light. Remember, that important factors that can be influenced BY the immune-system, but also have impact ON the immune-system include: -* Sleep -* Nutrition -* Stress disorders -* Malign diseases in the patients´ history -* Infections -* among others

You don’t have to be a psychologist or a specialist in nutrition, but you have to recognize that stressors can be signs of a maladaptive working neuro-immune-system. Clinicians must build a network of specialists in this area and foster communicate. If you treat or manage patients with chronic, especially neuropathic, pain disorders there are many other parameters to consider in addition to pain-threshold and movement dysfunctions. The mature organism model, used in many of the courses offered by Myopain Seminars, including the CRAFTA courses, gives us a nice guideline to think into this direction.
Clinical Implications
What are the clinical implications for the treatment of head and facial pain? Do we need some kind of paradigm shift, leading to a more multimodal management of chronic head and facial pain states? Does it require a broader understanding in acute situations?
The therapist’s clinical reasoning process should include an understanding of influencing factors for the patients’ situations, which implies that asking patients about their eating habits, sleep patterns is important possible with the addition of psychosocial screening tools. Therapists must develop excellent communication and empathic social skills. The challenge is to guide each patient through his or her unique situation and to practice from a self-reflective approach.
Often, it is useful treating patients with endurance training, strengthening exercises, or neurodynamic movements for the whole neuraxis (SLUMP movements etc.). Many applied, sometimes non-specific, techniques have several effect-mechanisms. Always be aware that every intervention has multifactorial effects, such as mechanical, neuro-immuno-physiological or psychological factors. Remember to always treat the human coming to your office and not a diagnosis or MRI scan!
Literature:
Allianz chronischer Schmerz. (2018). Allianz chronischer Schmerz Österreich. Retrieved February 21, 2018, from https://www.schmerz-allianz.at/
Gifford, L. (2014). Aches and Pains. CNS Press Ltd., Kestresl, Swanpool, Falmouth, Cornwall, TR11 5BD, UK. Haydon, P. G. (2001). GLIA: listening and talking to the synapse. Nature Reviews. Neuroscience, 2(3), 185–193. https://doi.org/10.1038/35058528
Milligan, E. D., & Watkins, L. R. (2009). Pathological and protective roles of glia in chronic pain. Nature Reviews. Neuroscience, 10(1), 23–36. https://doi.org/10.1038/nrn2533
Tracey, K. J. (2009). Reflex control of immunity. Nature Reviews. Immunology, 9(6), 418–428. https://doi.org/10.1038/nri2566