Many experts agree: exercise is a key component of chronic pain rehabilitation programs. Ideally, exercise may improve function and mood and in the longer term, exercise can provide relief of pain even in chronic pain populations (Meeus et al 2010, Friden et al 2013). But, sometimes that is easier said than done. Exercise may have little or no effect in patients with chronic or persistent pain and in some cases, exercise may even increase the pain experience by activating descending facilitatory mechanisms of the central nervous system (Knauf and Koltyn 2014, Van Oosterwijck et al 2012). This blog is based mostly on a recent article by Dommerholt, Mayberry, and Sickel (Dommerholt et al 2019) published in the German journal Der Schmerzpatient (The Pain Patient).
In healthy subjects, exercising typically reduces pain for about 30 minutes which is attributed to exercise-induced hypoalgesia (EIH) (Hoffman et al 2004, Vaegter et al 2014), but in chronic pain populations, the reliability of the EIH response is often poor (Vaegter et al 2019). Patients with widespread pain often present with local and global dysfunction of the EIH. An example of a local dysfunctional EIH may be seen in a patient with knee osteoarthritis and an impaired EIH when trying to perform lower extremity strengthening, but with a normal EIH when training the upper extremity (Rice et al 2019).
An impaired EIH may be more common in persons with augmented central nociceptive processing, but it is not entirely clear what mechanisms contribute to impaired EIH in chronic pain populations. Gender and psychological factors do not appear to be strongly linked to impaired EIH (Ickmans et al 2017, Hoeger Bement et al 2011), but dysfunctions of the immune system (Light et al 2009), the endocannabinoid system (Ghafouri et al 2013), and the autonomic nervous system (Barakat et al 2012)have been implicated. Kinesiophobia and pain catastrophizing may also play significant roles (Priore et al 2019, Coronado et al 2015). Kinesiophobic beliefs may alter a person’s pain intensity, but they appear to have little influence on EIH in patients with chronic musculoskeletal pain (Vaegter et al 2018). Pain catastrophizing is a strong predictor of poor outcomes in individuals with pain (Feinstein et al 2017).
Exercise programs that decrease the pain threshold and increase the pain experience will likely have a negative impact on the patient’s motivation and enthusiasm, furthering physical deconditioning, depression, and poor self-efficacy (Jack et al 2010). This can create a challenge for clinicians, who are expected to develop appropriate exercise programs without having reliable and objective parameters (Van Oosterwijck et al 2012, Daenen et al 2015). Physical therapists may be tempted to base the level of exercise programs for chronic pain patients on their fitness levels, but this may actually be counterproductive (Nijs et al 2012). There is some evidence that combining exercise programs with manual therapy, myofascial therapy, electrotherapy, and dry needling may provide greater pain relief during activity than exercise alone, although according to other studies, combination therapies may not always yield better results.
Combining exercise programs with neuroscience education may decrease pain and pain catastrophizing and improve function and physical performance. Patients may anticipate less pain with exercise and increase their confidence. Pain neuroscience education targets central nervous system dysfunction and potential peripheral sources of nociceptive input, and motor control issues.
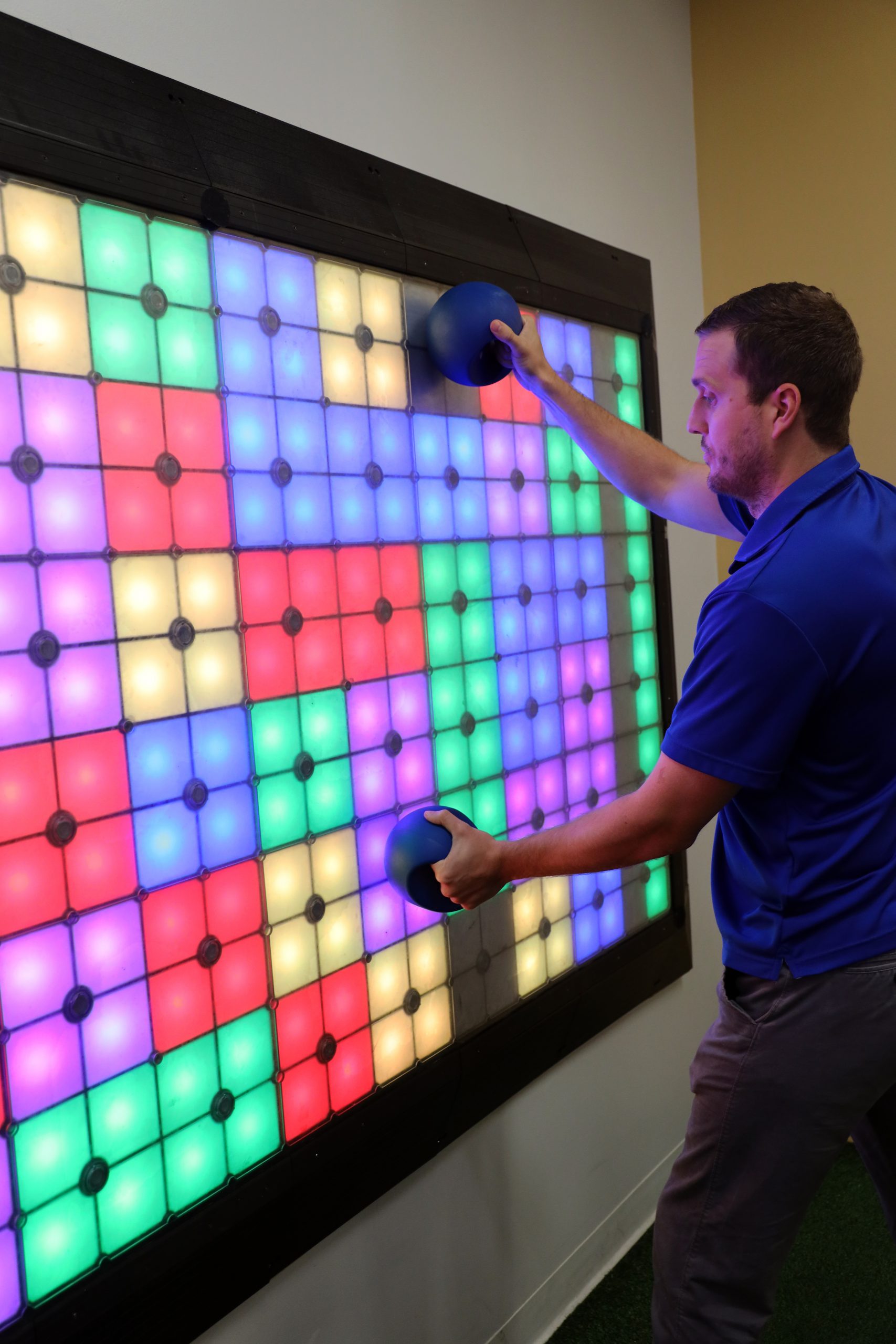
 External-focus exercise by itself is not a new concept and is commonly used within pediatric and neurologic physiotherapy; however, in the context of pain management programs, very few clinicians use an external focus of attention as part of a comprehensive treatment plan. Where an internal-focus approach is directed at the patient’s own body movements reflected in the directions the therapist will give to the patient, i.e., “place your right foot here, bend your knee and turn your trunk to the left,” which is body-focused language, an external-focus approach is always directed at the effects that a patient’s movements will have on the immediate environment. With an external focus, patients may be instructed to stand on an unstable surface, while hitting flashing lights with a stick.
External-focus exercise by itself is not a new concept and is commonly used within pediatric and neurologic physiotherapy; however, in the context of pain management programs, very few clinicians use an external focus of attention as part of a comprehensive treatment plan. Where an internal-focus approach is directed at the patient’s own body movements reflected in the directions the therapist will give to the patient, i.e., “place your right foot here, bend your knee and turn your trunk to the left,” which is body-focused language, an external-focus approach is always directed at the effects that a patient’s movements will have on the immediate environment. With an external focus, patients may be instructed to stand on an unstable surface, while hitting flashing lights with a stick.
The therapist’s objective of the activity may be improving trunk stabilization, upper extremity strengthening, and reducing kinesiophobia. The instructions to the patient do not include any body-focused language but are directed exclusively at the target. Perhaps perplexing, seemingly minor differences in instructions can make enormous differences in the patient’s learning potential. Avoiding any “body language” has consistently resulted in greater improvements in motor performance, i.e., instead of using “your feet” consider saying “your shoes”; instead of “doing a pelvic tilt” consider something like “move your belt buckle” (Liao and Masters 2001).
There is much evidence that adopting such an external focus facilitates unconscious and reflexive processes, which 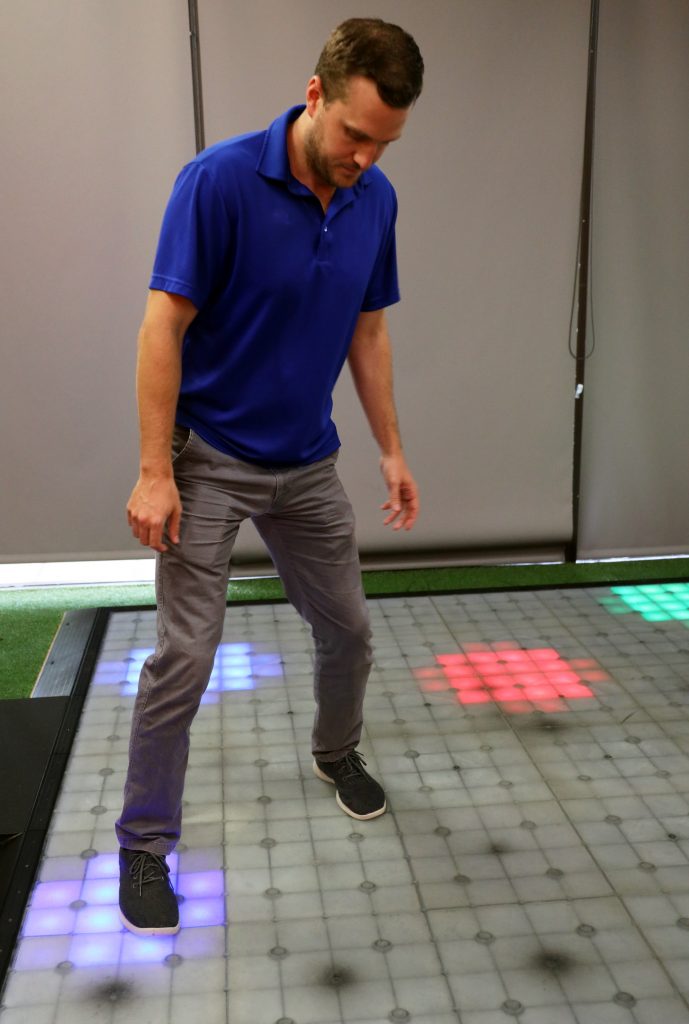 allows patients to gain control over their movement patterns and motor planning, and at the same time come to realize that they were able to move and complete a variety of tasks without an exacerbation of pain. While the patient may experience exercise as a fun and exciting activity, the desired results are more or less achieved without conscious awareness (Wulf and Su 2007, Wulf et al 2004). It is conceivable that external-focus exercise may trigger EIH, but there are no studies to support or refute this notion.
allows patients to gain control over their movement patterns and motor planning, and at the same time come to realize that they were able to move and complete a variety of tasks without an exacerbation of pain. While the patient may experience exercise as a fun and exciting activity, the desired results are more or less achieved without conscious awareness (Wulf and Su 2007, Wulf et al 2004). It is conceivable that external-focus exercise may trigger EIH, but there are no studies to support or refute this notion.
Target-focused therapy appears to improve patient compliance (Gangatharam 2018) and has many other benefits. In contrast to a cognition-targeted approach, patients are not asked to confront their own fears, as this strategy constitutes an internal focus approach. Instead, through participating in a wide variety of challenging activities with an external focus, patients will quickly realize that their functional capacity is far beyond their expectations without experiencing pain with movement and without having to assume an introspective, internal-focus position (Badami et al 2012). Lohse et al. maintained that an internal-focus approach may actually hinder learning new motor skills compared to an external-focus approach, which does not only improve motor performance but could also improve learning in general (Lohse et al 2014). An external-focus approach increases the automaticity of motor control without having to confront patients with their internalized fears (Lohse 2012, Totsika and Wulf 2003).
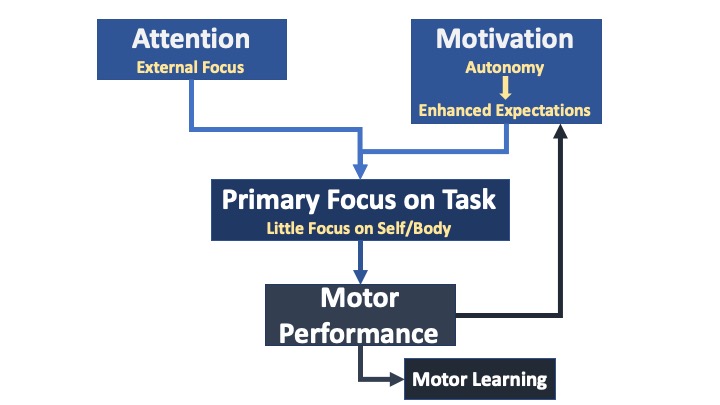 After more than twenty years of research in external-focus exercise and attentional learning, in 2016, Wulf and Lewthwaite defined the OPTIMAL Theory of Motor, where OPTIMAL is an acronym for Optimizing Performance Through Intrinsic Motivation and Attention for Learning (Wulf and Lewthwaite 2016). The newly defined motor learning theory includes the essential features of an external-focus exercise approach, incorporates the social-cognitive–affective–motor nature of “motor” behavior, and recognizes that motivation, attention, motor performance, and motor learning are intrinsically associated with each other (Lewthwaite and Wulf 2010). Motivational factors are an important aspect of the OPTIMAL theory and by default, of external-focus exercise.
After more than twenty years of research in external-focus exercise and attentional learning, in 2016, Wulf and Lewthwaite defined the OPTIMAL Theory of Motor, where OPTIMAL is an acronym for Optimizing Performance Through Intrinsic Motivation and Attention for Learning (Wulf and Lewthwaite 2016). The newly defined motor learning theory includes the essential features of an external-focus exercise approach, incorporates the social-cognitive–affective–motor nature of “motor” behavior, and recognizes that motivation, attention, motor performance, and motor learning are intrinsically associated with each other (Lewthwaite and Wulf 2010). Motivational factors are an important aspect of the OPTIMAL theory and by default, of external-focus exercise.
To learn more about external-focus exercise, consider attending the Playground Approach course offered by Eureka Seminars.
References
Badami, R, Vaezmousavi, M, Wulf, G & Namazizadeh, M, 2012. Feedback about more accurate versus less accurate trials: differential effects on self-confidence and activation. Research Quarterly for Exercise and Sport, 83, 196-203.
Barakat, A, Vogelzangs, N, Licht, CM, Geenen, R, Macfarlane, GJ, De Geus, EJ, Smit, JH, Penninx, BW & Dekker, J, 2012. Dysregulation of the autonomic nervous system and its association with the presence and intensity of chronic widespread pain. Arthritis Care Res (Hoboken), 64, 1209-1216.
Coronado, RA, George, SZ, Devin, CJ, Wegener, ST & Archer, KR, 2015. Pain Sensitivity and Pain Catastrophizing Are Associated With Persistent Pain and Disability After Lumbar Spine Surgery. Archives of Physical Medicine and Rehabilitation, 96, 1763-1770.
Daenen, L, Varkey, E, Kellmann, M & Nijs, J, 2015. Exercise, not to exercise, or how to exercise in patients with chronic pain? Applying science to practice. Clinical Journal of Pain, 31, 108-114.
Dommerholt, J, Mayberry, N & Sickel, M, 2019. Physiotherapie mit externem Fokus. Der Schmerzpatient, 2, 178-187.
Feinstein, AB, Sturgeon, JA, Darnall, BD, Dunn, AL, Rico, T, Kao, MC & Bhandari, RP, 2017. The Effect of Pain Catastrophizing on Outcomes: A Developmental Perspective Across Children, Adolescents, and Young Adults With Chronic Pain. J Pain, 18, 144-154.
Friden, C, Thoors, U, Glenmark, B, Kosek, E, Nordmark, B, Lundberg, IE & Opava, CH, 2013. Higher pain sensitivity and lower muscle strength in postmenonpausal women with early rheumatoid arthritis compared with age-matched healthy women–a pilot study. Disability and Rehabilitation, 35, 1350-1356.
Gangatharam, S, 2018. Target-focused exercise regime to improve patient compliance and range of motion in the stiff hand. Journal of Hand Therapy, 31, 568-571.
Ghafouri, N, Ghafouri, B, Larsson, B, Stensson, N, Fowler, CJ & Gerdle, B, 2013. Palmitoylethanolamide and stearoylethanolamide levels in the interstitium of the trapezius muscle of women with chronic widespread pain and chronic neck-shoulder pain correlate with pain intensity and sensitivity. Pain, 154, 1649-1658.
Hoeger Bement, MK, Weyer, A, Hartley, S, Drewek, B, Harkins, AL & Hunter, SK, 2011. Pain perception after isometric exercise in women with fibromyalgia. Archives of Physical Medicine and Rehabilitation, 92, 89-95.
Hoffman, MD, Shepanski, MA, Ruble, SB, Valic, Z, Buckwalter, JB & Clifford, PS, 2004. Intensity and duration threshold for aerobic exercise-induced analgesia to pressure pain. Archives of Physical Medicine and Rehabilitation, 85, 1183-1187.
Ickmans, K, Malfliet, A, De Kooning, M, Goudman, L, Hubloue, I, Schmitz, T, Goubert, D & Aguilar-Ferrandiz, ME, 2017. Lack of Gender and Age Differences in Pain Measurements Following Exercise in People with Chronic Whiplash-Associated Disorders. Pain Physician, 20, E829-E840.
Jack, K, Mclean, SM, Moffett, JK & Gardiner, E, 2010. Barriers to treatment adherence in physiotherapy outpatient clinics: a systematic review. Man Ther, 15, 220-228.
Knauf, MT & Koltyn, KF, 2014. Exercise-induced modulation of pain in adults with and without painful diabetic neuropathy. J Pain, 15, 656-663.
Lewthwaite, R & Wulf, G, 2010. Grand challenge for movement science and sport psychology: embracing the social-cognitive-affective-motor nature of motor behavior. Front Psychol, 1, 42.
Liao, CM & Masters, RS, 2001. Analogy learning: a means to implicit motor learning. Journal of Sports Sciences, 19, 307-319.
Light, AR, White, AT, Hughen, RW & Light, KC, 2009. Moderate exercise increases expression for sensory, adrenergic, and immune genes in chronic fatigue syndrome patients but not in normal subjects. J Pain, 10, 1099-1112.
Lohse, KR, 2012. The influence of attention on learning and performance: pre-movement time and accuracy in an isometric force production task. Hum Mov Sci, 31, 12-25.
Lohse, KR, Sherwood, DE & Healy, AF, 2014. On the advantage of an external focus of attention: a benefit to learning or performance? Hum Mov Sci, 33, 120-134.
Meeus, M, Roussel, NA, Truijen, S & Nijs, J, 2010. Reduced pressure pain thresholds in response to exercise in chronic fatigue syndrome but not in chronic low back pain: an experimental study. J Rehabil Med, 42, 884-890.
Nijs, J, Kosek, E, Van Oosterwijck, J & Meeus, M, 2012. Dysfunctional endogenous analgesia during exercise in patients with chronic pain: to exercise or not to exercise? Pain Physician, 15, ES205-213.
Priore, LB, Azevedo, FM, Pazzinatto, MF, Ferreira, AS, Hart, HF, Barton, C & De Oliveira Silva, D, 2019. Influence of kinesiophobia and pain catastrophism on objective function in women with patellofemoral pain. Phys Ther Sport, 35, 116-121.
Rice, D, Nijs, J, Kosek, E, Wideman, T, Hasenbring, MI, Koltyn, K, Graven-Nielsen, T & Polli, A, 2019. Exercise-Induced Hypoalgesia in Pain-Free and Chronic Pain Populations: State of the Art and Future Directions. J Pain, 20, 1249-1266.
Totsika, V & Wulf, G, 2003. The influence of external and internal foci of attention on transfer to novel situations and skills. Research Quarterly for Exercise and Sport, 74, 220-225.
Vaegter, HB, Handberg, G & Graven-Nielsen, T, 2014. Similarities between exercise-induced hypoalgesia and conditioned pain modulation in humans. Pain, 155, 158-167.
Vaegter, HB, Lyng, KD, Yttereng, FW, Christensen, MH, Sorensen, MB & Graven-Nielsen, T, 2019. Exercise-Induced Hypoalgesia After Isometric Wall Squat Exercise: A Test-Retest Reliabilty Study. Pain Med, 20, 129-137.
Vaegter, HB, Madsen, AB, Handberg, G & Graven-Nielsen, T, 2018. Kinesiophobia is associated with pain intensity but not pain sensitivity before and after exercise: an explorative analysis. Physiotherapy, 104, 187-193.
Van Oosterwijck, J, Nijs, J, Meeus, M, Van Loo, M & Paul, L, 2012. Lack of endogenous pain inhibition during exercise in people with chronic whiplash associated disorders: an experimental study. J Pain, 13, 242-254.
Wulf, G & Lewthwaite, R, 2016. Optimizing performance through intrinsic motivation and attention for learning: The OPTIMAL theory of motor learning. Psychon Bull Rev, 23, 1382-1414.
Wulf, G, Mercer, J, Mcnevin, N & Guadagnoli, MA, 2004. Reciprocal influences of attentional focus on postural and suprapostural task performance. J Mot Behav, 36, 189-199.
Wulf, G & Su, J, 2007. An external focus of attention enhances golf shot accuracy in beginners and experts. Research Quarterly for Exercise and Sport, 78, 384-389.