Initial Examination of Lower Back Pain
As a clinician, you may have seen patients with a history of long-term or recurring low back pain. When you conduct your initial examination, they may tell you that “It’s been a few weeks, and my pain has not gone away. I have rested, taken anti-inflammatories, done stretches, and tried some exercises I found on the internet, but nothing seems to have helped.”
When you question the patient about the nature and location of the pain, they may report that they have a dull ache in the lower back that makes it difficult to sit for prolonged periods of time. The pain is worse when they try to work out, and it even moves into the outside of the hip and sometimes sends a stabbing pain into the pelvic area. They may have seen other clinicians who gave them exercise programs, but they had difficulty tolerating the exercises and ended up in more pain [1].
How Lower Back Pain Effects Pelvic Floor Dysfunction
One study showed that 95% of women with a complaint of low back / pelvic pain also had pelvic floor dysfunction [2]. Perhaps what has been missing from their previous treatment plan is a thorough exploration of what peripheral sources of nociceptive input may be involved, including the pelvic floor. Pelvic floor therapists would likely have examined the patient in more detail, but more generic therapists may not always be aware that pelvic floor dysfunction can cause or contribute to low back pain.
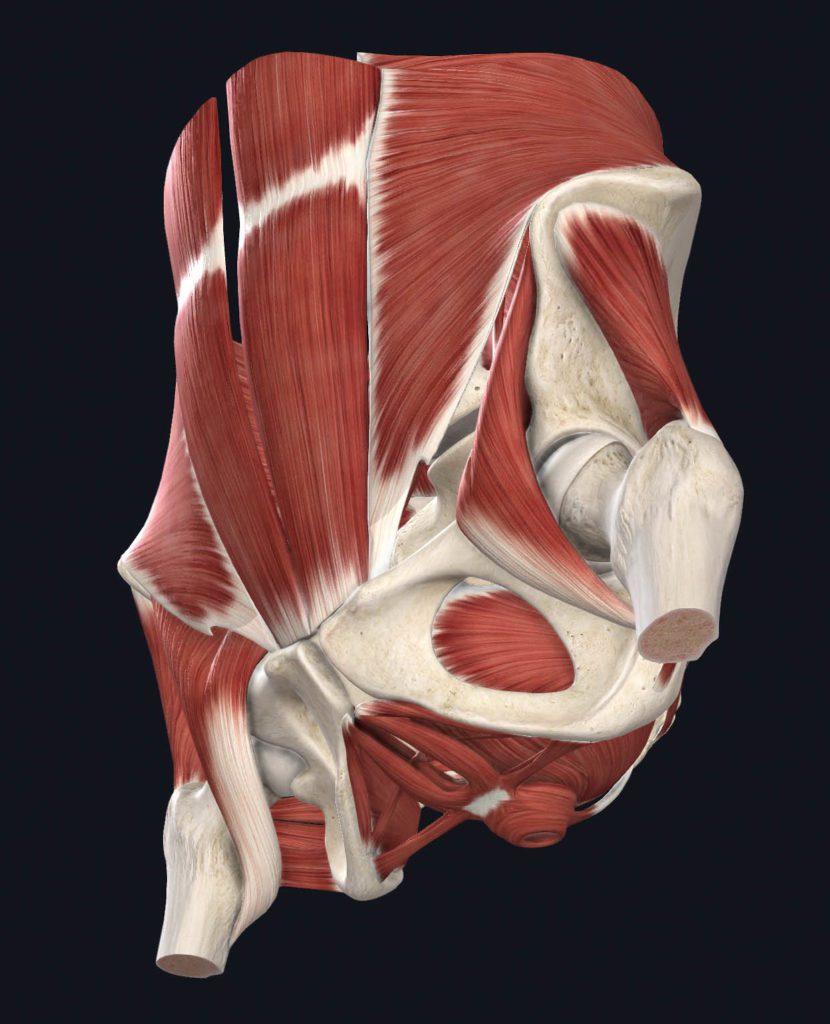
The Muscles of the Pelvic Floor
Fun fact: The muscles of the pelvic floor not only control urinary and sexual function, but they also play a role in core control. They are part of a group of muscles that includes the deep abdominals, deep lower back muscles, and diaphragm. When there is an injury or pain associated with one of these muscles, the others are likely involved.
In the case of lower back pain, a patient may also deal with coccydynia and pelvic floor dysfunction. Believe it or not, there is a greater association between low back pain and pelvic floor dysfunction than obesity or inactivity.
Addressing Chronic Pelvic Pain in Men and Women
The American College of Obstetricians and Gynecologists specifies the location of chronic pelvic pain or CPP in the pelvis, the abdominal wall at or below the umbilicus, lumbar, sacral, and buttock regions [3]. Approximately 90% of women with pelvic pain, interstitial cystitis, or incontinence have painful trigger points in several locations, including the pelvic floor, gluteal and abdominal muscles [4-6]. The prevalence of CPP is estimated to be 14.7% of women between 18–50 years of age in the USA [7].
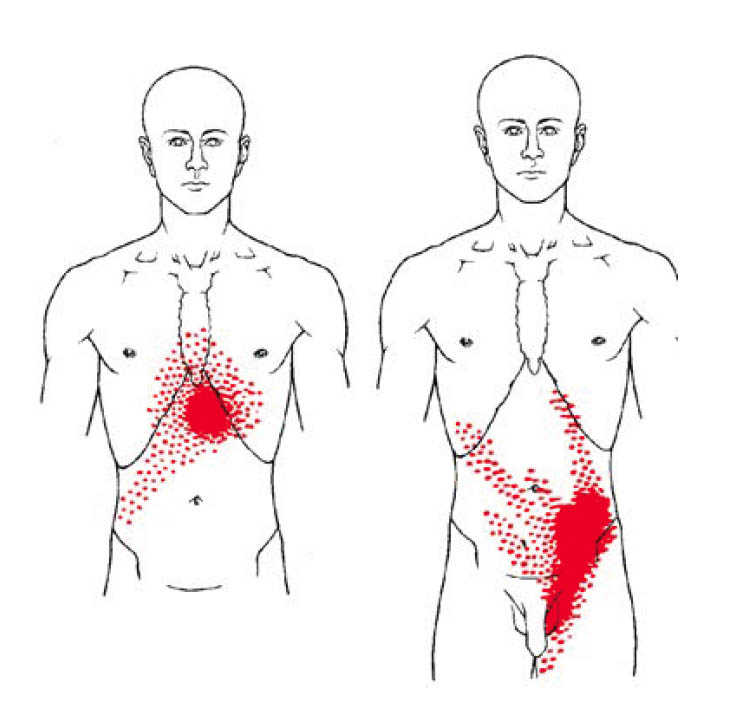 Men with chronic prostatitis (CP) and chronic pelvic pain syndrome (CPPS) presented with pain in the scrotal, perineal, inguinal, and bladder area in 54% of cases and had tender myofascial palpation in 88% of cases [8]. Berger et al. noted that in men with CPPS, the pain was not always limited to the prostate [9], and often involved the external and internal pelvic floor and the suprapubic area [10]. Abdominal or pelvic tenderness was present in half of the patients with chronic pelvic pain syndrome but only in 7% of controls [10]. Anderson et al. further reported that puborectalis, pubococcygeus, and rectus abdominus TrPs reproduced penile pain 75% of the time, and external oblique TrPs elicited suprapubic, groin, and testicular pain in 80% of the cases [11].
Men with chronic prostatitis (CP) and chronic pelvic pain syndrome (CPPS) presented with pain in the scrotal, perineal, inguinal, and bladder area in 54% of cases and had tender myofascial palpation in 88% of cases [8]. Berger et al. noted that in men with CPPS, the pain was not always limited to the prostate [9], and often involved the external and internal pelvic floor and the suprapubic area [10]. Abdominal or pelvic tenderness was present in half of the patients with chronic pelvic pain syndrome but only in 7% of controls [10]. Anderson et al. further reported that puborectalis, pubococcygeus, and rectus abdominus TrPs reproduced penile pain 75% of the time, and external oblique TrPs elicited suprapubic, groin, and testicular pain in 80% of the cases [11].
Giamberardino et al. reported that patients with visceral pain and hyperalgesia are likely to have clinically relevant abdominal TrPs [12 13]. Myofascial pain was identified in 78.5% of patients with interstitial cystitis, and 67.9% of those patients had six or more identifiable TrPs. The most common TrPs were found in the obturator internus, puborectalis, arcus tendineus and iliococcygeus muscles [14].
Treating Pelvic Floor Dysfunction
Treating pelvic floor dysfunction associated with lower back pain may involve many interventions, including trigger point dry needling for pelvic pain, pelvic floor internal pain release, and appropriate exercises to target relaxation of the muscles associated with the low back and pelvic regions.
If you are unfamiliar with these treatment options, consider attending the Myopain Seminars pelvic pain and dysfunction courses and the Dry Needling for Pelvic Pain course.
Blair Green, PT, DPT, OCS, PHC
Myopain Seminars: Dry Needling for Pelvic Pain
Myopain Seminars offers a variety of dry needling courses specifically designed for different areas of the body. Our Dry Needling for Pelvic Pain course is designed with the pelvic health practitioner in mind. It improves the proficiency of dry needling skills in these providers while maintaining focus on the muscles most commonly treated in people with chronic pelvic pain and other types of pelvic floor dysfunction.
 This 3-day course will introduce the concepts of trigger point dry needling as it relates to the muscles of the pelvis and perineum. It will integrate pain science research with anatomy and biomechanics of the pelvis and pelvic floor.
This 3-day course will introduce the concepts of trigger point dry needling as it relates to the muscles of the pelvis and perineum. It will integrate pain science research with anatomy and biomechanics of the pelvis and pelvic floor.
Students will learn techniques to perform trigger point dry needling to the region safely. They will also learn clinical patterns that may facilitate improved clinical reasoning as to when and where to utilize trigger point dry needling. Muscle groups include the hip abductors, adductors, flexors, abdominal muscles, urogenital triangle, levator ani, and coccygeus. Students will review the anatomy, function, and dry needling techniques for each muscle.
Myopain offers courses across the globe, if you are interested in taking our Dry Needling for Pelvic Pain course, find a location near you.
References
- FitzGerald MP, Kotarinos R. Rehabilitation of the short pelvic floor. I: Background and patient evaluation. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2003;14(4):261-8
- Dufour S, Vandyken B, Forget MJ, Vandyken C. Association between lumbopelvic pain and pelvic floor dysfunction in women: A cross sectional study. Musculoskelet Sci Pract 2018;34:47-53
- Vercellini P, Somigliana E, Vigano P, Abbiati A, Barbara G, Fedele L. Chronic pelvic pain in women: etiology, pathogenesis and diagnostic approach. Gynecol. Endocrinol. 2009;25(3):149-58
- Weiss JM. Pelvic floor myofascial trigger points: manual therapy for interstitial cystitis and the urgency-frequency syndrome. J. Urol. 2001;166(6):2226-31
- FitzGerald MP, Kotarinos R. Rehabilitation of the short pelvic floor. II: Treatment of the patient with the short pelvic floor. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2003;14(4):269-75
- Warren JW, Langenberg P, Greenberg P, Diggs C, Jacobs S, Wesselmann U. Sites of pain from interstitial cystitis/painful bladder syndrome. J. Urol. 2008;180(4):1373-7
- Mathias SD, Kuppermann M, Liberman RF, Lipschutz RC, Steege JF. Chronic pelvic pain: prevalence, health-related quality of life, and economic correlates. Obstet. Gynecol. 1996;87(3):321-7
- Zermann DH, Ishigooka M, Doggweiler R, Schmidt RA. Chronic prostatitis: a myofascial pain syndrome? Infect Urol 1999;12(3):84-92
- Berger RE, Ciol MA, Rothman I, Turner JA. Pelvic tenderness is not limited to the prostate in chronic prostatitis/chronic pelvic pain syndrome (CPPS) type IIIA and IIIB: comparison of men with and without CP/CPPS. BMC Urol 2007;7:17
- Shoskes DA, Berger R, Elmi A, Landis JR, Propert KJ, Zeitlin S. Muscle tenderness in men with chronic prostatitis/chronic pelvic pain syndrome: the chronic prostatitis cohort study. J. Urol. 2008;179(2):556-60
- Anderson RU, Sawyer T, Wise D, Morey A, Nathanson BH. Painful myofascial trigger points and pain sites in men with chronic prostatitis/chronic pelvic pain syndrome. The Journal of urology 2009;182(6):2753-8
- Giamberardino MA, Affaitati G, Iezzi S, Vecchiet L. Referred muscle pain and hyperalgesia from viscera. J Musculoskeletal Pain 1999;7(1/2):61-69
- Giamberardino MA, Vecchiet L. Visceral pain, referred hyperalgesia and outcome: new concepts. Eur. J. Anaesthesiol. Suppl. 1995;10:61-6
- Bassaly R, Tidwell N, Bertolino S, Hoyte L, Downes K, Hart S. Myofascial pain and pelvic floor dysfunction in patients with interstitial cystitis. Int Urogynecol J 2011;22(4):413-8
Dry Needling Course Series
The Dry Needling 1 course is an excellent starting point for learning the fundamentals of dry needling therapy. With a focus on the safe and effective application of dry needling techniques, you will gain a solid understanding of myofascial trigger points, needling techniques, precautions, and how to apply these techniques in clinical practice.
The Dry Needling 2 course is an intermediate-level course that provides in-depth knowledge and hands-on training for dry needling techniques of the extremities, including the upper and lower body. By completing this course, you will expand upon the skills you acquired in the DN-1 course and better understand the application of dry needling for managing musculoskeletal pain and dysfunction.
The Dry Needling 3 course is the final course in the series and the last step before becoming a Certified Myofascial Trigger Point Therapist – Dry Needling (CMTPT/DN). This course offers an in-depth study of advanced dry needling techniques for hand muscles, several lower extremity and foot muscles, the craniofacial and craniomandibular muscles, and more.