Intramuscular Electrical Stimulation
Busy clinicians and patients with chronic pain are searching for treatment options that are safe, inexpensive, and effective. In the pain medicine and rehabilitation fields, neuromodulation is increasingly used as a safer alternative to medications for the management of pain (Reuter et al., 2019).
Neuromodulation is the delivery of electrical stimuli to the body to alter neural pathways peripherally or centrally for therapeutic effect
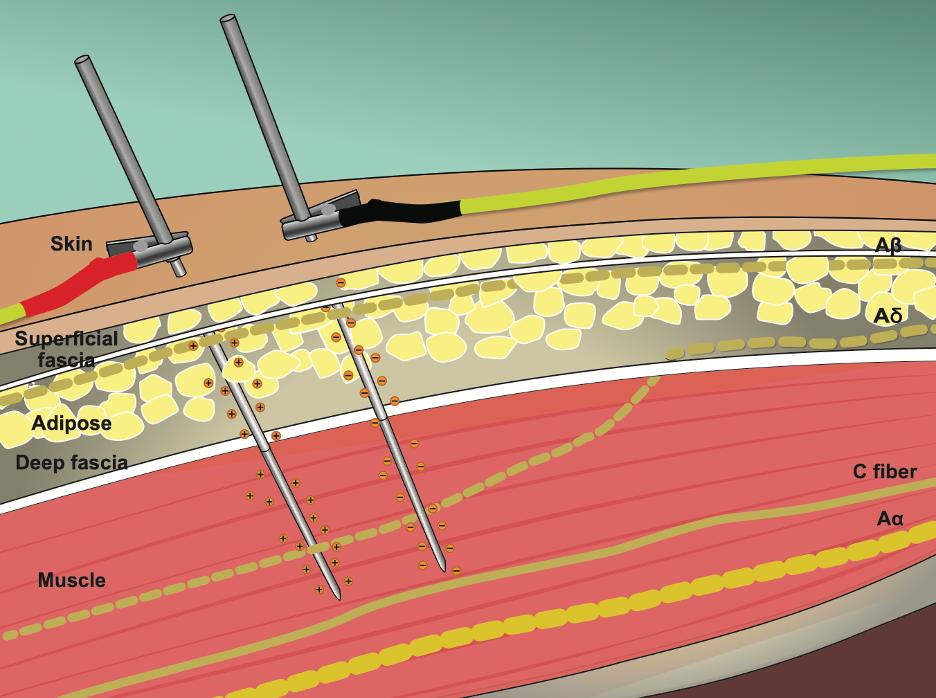
Neuromodulation consists of both central and peripheral nerve stimulation techniques that involve invasive and non-invasive methods (Ginn et al., 2019). Electrotherapy has been administered for decades by clinicians as a form of peripheral nerve stimulation (PNS) to reduce pain and improve motor function using Transcutaneous Electrical Nerve Stimulation (TENS) (Vance et al., 2022) and Neuromuscular Electrical Stimulation (NMES) modalities (Happ & Behringer, 2022), respectively. Both TENS and NMES deliver electrical pulses through cutaneous electrodes to stimulate large-diameter nerve fibers.
More recently, percutaneous techniques have been incorporated into clinical practice, which involves electrical stimulation to indwelling needles for the treatment of patients with acute and chronic pain (Plaza-Manzano et al., 2020; Hadizadeh et al., 2021), similar to the practice of electroacupuncture (Lv et al., 2019) but with differences in the underlying theory (Cummings, 2001). These forms of neuromodulation are less invasive, as they do not require surgically implanted electrodes or implanted electrical devices.
A recent systematic review supports both electrical stimulation modalities with surface electrodes and percutaneous approaches but was unable to validate which approach was superior in the treatment of pain conditions (Beltran-Alacreu et al., 2022).
Recent studies found that electrical stimulation techniques using needles are effective in the treatment of myofascial pain (Ahmed et al., 2019) and in reducing pain across a wide range of musculoskeletal conditions such as lower back pain, knee osteoarthritis, plantar heel pain, and neck pain (Plaza-Manzano et al., 2020).
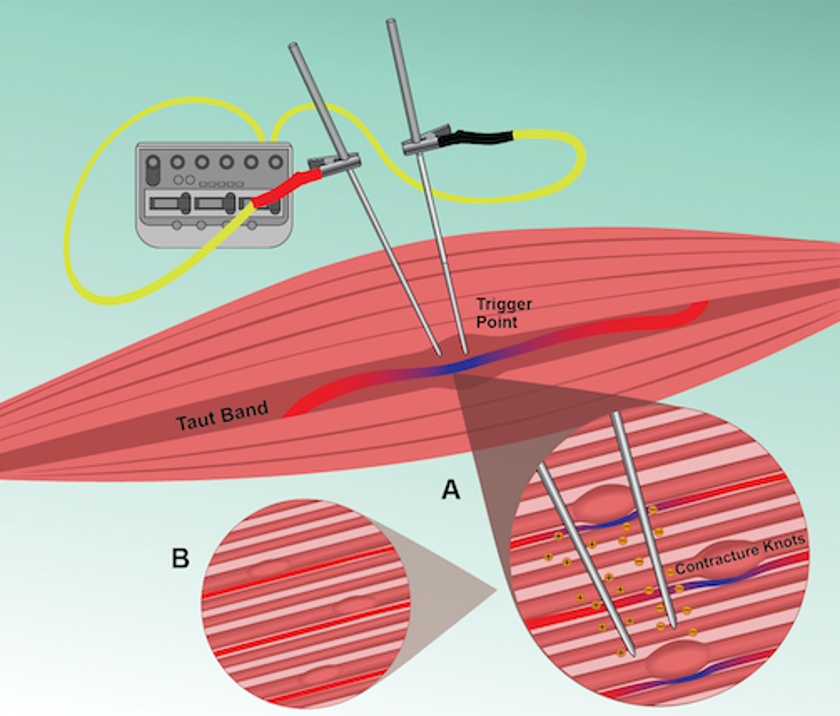
Intramuscular electrical stimulation (IMES) is a technique that delivers electrical current through needles inserted into muscles and, more precisely, into trigger points. According to a recent scoping review, when IMES is used to target trigger points, it reduces endplate noise, normalizes muscle blood flow, and elicits antinociceptive effects by engaging the dorsal periaqueductal gray and descending pain inhibitory systems (Perreault et al., 2022).
Another feature of IMES of interest to clinicians and patients is that the added electrical current has the potential to elicit local twitch responses with less local muscle injury, inflammatory reactions, and post-needling soreness that can accompany dry needling when only repeated needle manipulation is used (Perreault et al., 2017; Margalef et al., 2020). León-Hernández and colleagues (2016) reported that the use of percutaneous electrical stimulation following dry needling to trigger points in patients with chronic neck pain led to greater pain reduction and less post-needling soreness compared to dry needling alone.
In clinical settings, electrical current is delivered by a charge-generating stimulator, such as an electro-acupuncture device or a TENS unit. Pulses from the charge generator direct the flow of current by pushing streams of free electrons through a small fine wire conductor down the shaft of an inserted needle. The charge’s influence at the needle’s tip will depend on its proximity to nerve endings and the amount of electrical charge delivered.

A symmetrical biphasic waveform is commonly used with either square or rectangular waves split into two phases: a negative charge delivered via a cathode, followed by a positive charge delivered through an anode. Ultimately, the objective is to use electrical charge delivered through needles to alter the membrane potential around nerves to stimulate afferent activity or elicit motor responses.
A recent scoping review of clinical trials was unable to determine if certain dosage variables of dry needling impact pain outcomes due to inconsistencies with the reporting of dry needling parameters (Kearns et al., 2023). Likewise, systematic reviews have been unable to conclude which specific parameters of electrical stimulation contribute to superior outcomes in clinical trials. This is especially the case with IMES and the selection of electrical stimulation parameters.
Until now, Myopain Seminars has resisted including IMES in our dry needling courses simply because there just was not enough scientific evidence. We believe that most IMES “protocols” promoted in other courses are just empirical concepts without much scientific validity. While that may be OK, especially when followed by research exploring the mechanisms and clinical outcomes, in reality, very few course programs conduct high-quality research in the area of IMES but are happy to present applications based on somewhat dubious low-quality research.
No published guidelines are available to assist clinicians in selecting the optimal IMES parameters
Navigating the literature to understand IMES better and its various applications and parameters is difficult for busy clinicians due to the high volume of new research, empirically driven practice patterns, inconsistencies in terminology, and the overlap with other electricity-based interventions, such as electroacupuncture (EA). In addition, very few courses are available that teach the proper theory and clinical application of IMES.
Myopain Seminars has created a new online course on Intramuscular Electrical Stimulation to meet this need. While creating this course, we conducted several IMES studies, including a clinical outcomes study (Hadizadeh et al., 2021) and an IMES mechanism study (Perreault et al., 2022), which, once again, makes Myopain Seminars the obvious choice!
The new IMES course was created to teach clinicians how to implement IMES safely and effectively in practice. Students will learn the best available clinical and experimental research on electricity-based needling interventions in an interesting format with immediate applicability. Learners will have access to audio-visual presentations, practical instructional videos, article summaries, reading assignments, and label illustrations to accommodate many preferred learning styles.
Tommy Perreault and Jan Dommerholt
Intramuscular electrical stimulation (IMES) is increasingly used in clinical practice to modify or enhance the effects of needling interventions. Yet, no published guidelines exist to assist clinicians in their clinical reasoning for selecting stimulation parameters or determining adequate dosage for the use of IMES for any musculoskeletal condition. This online course will teach clinicians how to safely and effectively implement IMES into practice based on the most recent scientific evidence.
References
Ahmed, S., Haddad, C., Subramaniam, S., Khattab, S., & Kumbhare, D. (2019). The Effect of Electric Stimulation Techniques on Pain and Tenderness at the Myofascial Trigger Point: A Systematic Review. Pain Med, 20(9), 1774-1788. https://doi.org/10.1093/pm/pny278
Beltran-Alacreu, H., Serrano-Muñoz, D., Martín-Caro Álvarez, D., Fernández-Pérez, J. J., Gómez-Soriano, J., & Avendaño-Coy, J. (2022). Percutaneous Versus Transcutaneous Electrical Nerve Stimulation for the Treatment of Musculoskeletal Pain. A Systematic Review and Meta-Analysis. Pain Med, 23(8), 1387-1400. https://doi.org/10.1093/pm/pnac027
Cummings, M. (2001). Percutaneous Electrical Nerve Stimulation – Electroacupuncture by Another Name? A Comparative Review. Acupuncture in Medicine, 19(1), 32-35. https://doi.org/10.1136/aim.19.1.32
Ginn, C., Patel, B., & Walker, R. (2019). Existing and emerging applications for the neuromodulation of nerve activity through targeted delivery of electric stimuli. Int J Neurosci, 129(10), 1013-1023. https://doi.org/10.1080/00207454.2019.1609473
Hadizadeh, M., Rahimi, A., Javaherian, M., Velayati, M., & Dommerholt, J. (2021). The efficacy of intramuscular electrical stimulation in the management of patients with myofascial pain syndrome: a systematic review. Chiropr Man Therap, 29(1), 40. https://doi.org/10.1186/s12998-021-00396-z
Happ, K. A., & Behringer, M. (2022). Neuromuscular Electrical Stimulation Training vs. Conventional Strength Training: A Systematic Review and Meta-Analysis of the Effect on Strength Development. J Strength Cond Res, 36(12), 3527-3540. https://doi.org/10.1519/jsc.0000000000004119
Kearns, G. A., Brismée, J. M., Riley, S. P., Wang-Price, S., Denninger, T., & Vugrin, M. (2023). Lack of standardization in dry needling dosage and adverse event documentation limits outcome and safety reports: a scoping review of randomized clinical trials. Journal of Manual & Manipulative Therapy, 31(2), 72–83. https://doi.org/10.1080/10669817.2022.2077516
León-Hernández, J. V., Martín-Pintado-Zugasti, A., Frutos, L. G., Alguacil-Diego, I. M., de la Llave-Rincón, A. I., & Fernandez-Carnero, J. (2016). Immediate and short-term effects of the combination of dry needling and percutaneous TENS on post-needling soreness in patients with chronic myofascial neck pain. Braz J Phys Ther, 20(5), 422-431. https://doi.org/10.1590/bjpt-rbf.2014.0176
Lv, Q., Wu, F., Gan, X., Yang, X., Zhou, L., Chen, J., . . . Liu, L. (2019). The Involvement of Descending Pain Inhibitory System in Electroacupuncture-Induced Analgesia. Front Integr Neurosci, 13, 38. https://doi.org/10.3389/fnint.2019.00038
Margalef, R., Bosque, M., Monclús, P., Flores, P., Minaya-Muñoz, F., Valera-Garrido, F., & Santafé, M. M. (2020). Percutaneous Application of Galvanic Current in Rodents Reverses Signs of Myofascial Trigger Points. Evidence-based Complementary and Alternative Medicine : eCAM, 2020, 4173218. https://doi.org/10.1155/2020/4173218
Perreault, T., Ball, A., Dommerholt, J., Theiss, R., Fernández-de-Las-Peñas, C., & Butts, R. (2022). Intramuscular Electrical Stimulation to Trigger Points: Insights into Mechanisms and Clinical Applications-A Scoping Review. J Clin Med, 11(20). https://doi.org/10.3390/jcm11206039
Perreault, T., Dunning, J., & Butts, R. (2017). The local twitch response during trigger point dry needling: Is it necessary for successful outcomes? J Bodyw Mov Ther, 21(4), 940-947. https://doi.org/10.1016/j.jbmt.2017.03.008
Plaza-Manzano, G., Gómez-Chiguano, G. F., Cleland, J. A., Arías-Buría, J. L., Fernández-de-Las-Peñas, C., & Navarro-Santana, M. J. (2020). Effectiveness of percutaneous electrical nerve stimulation for musculoskeletal pain: A systematic review and meta-analysis. Eur J Pain, 24(6), 1023-1044. https://doi.org/10.1002/ejp.1559
Reuter, U., McClure, C., Liebler, E., & Pozo-Rosich, P. (2019). Non-invasive neuromodulation for migraine and cluster headache: a systematic review of clinical trials. J Neurol Neurosurg Psychiatry, 90(7), 796-804. https://doi.org/10.1136/jnnp-2018-320113
Vance, C. G. T., Dailey, D. L., Chimenti, R. L., Van Gorp, B. J., Crofford, L. J., & Sluka, K. A. (2022). Using TENS for Pain Control: Update on the State of the Evidence. Medicina (Kaunas), 58(10). https://doi.org/10.3390/medicina58101332