Dry Needling for Multiple Sclerosis, Spinal Cord Injuries, & More
In the short history of dry needling, the focus of the vast majority of “dry needlers” has been on orthopedics and sports medicine. Recently, dry needling is increasingly used in the treatment of patients with spasticity, a common finding in patients with multiple sclerosis (65%), spinal cord injury (65%), and stroke (40-60%). Spasticity, according to Burridge et al. (2005), features “disordered sensory-motor control, resulting from an upper motor neuron lesion and presenting as intermittent or sustained involuntary activation of muscles” (Burridge et al. 2005). In our textbook “Trigger Point Dry Needling” (Dommerholt and Fernández De Las Peñas 2018), Jaime Salom Moreno and César Fernández de las Peñas describe that muscle contractures secondary to spasticity are commonly due to an increase in the number of cross-bridges, increased muscle stiffness and collagen tissue, and a decrease in muscle fiber length. It is known that dry needling damages the neuromuscular junction, which may at least partially explain the positive effects of dry needling on spasticity (Domingo et al. 2013).

Dry Needling Techniques for Muscles With Spasticity
Whereas dry needling for orthopedic problems is usually performed with the muscle in a relaxed position, with spasticity, it may be more beneficial to place the muscle in a slightly pre-stretched position. Twitch responses in spastic muscles often engage the entire muscle and are characterized as “global twitch responses (GTR).” Sometimes, GTRs occur in antagonistic muscles. Once the muscle tone is decreased, the muscle is stretched as much as feasible, and the dry needling is repeated in the new position.
Dry Needling vs. Acupuncture for Post-Stroke Spasticity
The evidence for the effects of dry needling is slowly growing. Already in 2007, Gallego and Mayoral described dry needling for quadriparesis of a 4-year-old child (Gallego and Mayoral 2007). This was one of the earliest case reports on dry needling to reduce spasticity. Around that same time, a few acupuncture studies described promising results (Mukherjee et al. 2007, Zhao et al. 2009), but others failed to detect significant improvements (Wayne et al. 2005, Fink et al. 2004). A more recent meta-analysis showed that acupuncture or electro-acupuncture could potentially reduce spasticity after stroke (Lim et al. 2015, Lim et al. 2017).
Studies on Dry Needling for Spasticity
Looking at dry needling studies, a Spanish study of 34 patients showed significant improvements in spasticity after a single session of dry needling into the medial and lateral gastrocnemius and anterior tibialis muscles. The outcome measures included the Modified Ashworth Scale, mechanical pain sensitivity with a pressure algometer to the second metacarpals, deltoid and anterior tibialis muscles bilaterally, and several baropodometric factors (Salom-Moreno et al. 2014). Several Iranian case reports and studies have also shown encouraging results. Ansari and colleagues published a case report in 2015 demonstrating reduced spasticity after dry needling the pronator teres, flexor carpi radialis, and flexor carpi ulnaris muscles (Ansari et al. 2015). In another study, 29 patients with a stroke received one session of dry needling to the flexor carpi radialis and flexor carpi ulnaris muscles, and again, dry needling contributed to a temporary reduction in spasticity and alpha motor neuron excitability (Fakhari et al. 2017).
Effects of Dry Needling on Stroke Patients With Spasticity
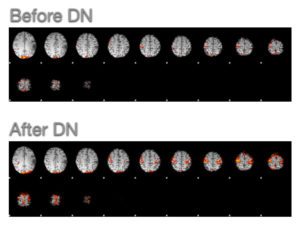 After several visits to Iran in 2017 and 2018, Myopain Seminars’ President, Dr. Jan Dommerholt, has collaborated multiple times with Dr. Noureddin Nakhostin Ansari and his team, resulting in the publication of several case reports and studies. Most recently, we shared the first neuroimaging study of the effect of dry needling on brain activity of a stroke patient with spasticity (Mohammadpour et al. 2020). Dry needling increased the activity in the affected primary motor cortex with motor improvement in a patient with post-stroke spastic hemiparesis. Functional magnetic resonance imaging revealed significant brain changes after dry needling indicating beneficial effects of dry needling for stroke patients with spasticity. In another study, we explored the effect of dry needling on lower limb dysfunction in 24 subjects (Ghannadi et al. 2020). While there were no changes in active range of motion, dry needling decreased muscle spasticity and improved lower limb function and gait speed. In a similar but still unpublished study, dry needling improved upper limb spasticity as measured by the Modified Modified Ashworth score, and increased passive wrist range of motion compared to controls.
After several visits to Iran in 2017 and 2018, Myopain Seminars’ President, Dr. Jan Dommerholt, has collaborated multiple times with Dr. Noureddin Nakhostin Ansari and his team, resulting in the publication of several case reports and studies. Most recently, we shared the first neuroimaging study of the effect of dry needling on brain activity of a stroke patient with spasticity (Mohammadpour et al. 2020). Dry needling increased the activity in the affected primary motor cortex with motor improvement in a patient with post-stroke spastic hemiparesis. Functional magnetic resonance imaging revealed significant brain changes after dry needling indicating beneficial effects of dry needling for stroke patients with spasticity. In another study, we explored the effect of dry needling on lower limb dysfunction in 24 subjects (Ghannadi et al. 2020). While there were no changes in active range of motion, dry needling decreased muscle spasticity and improved lower limb function and gait speed. In a similar but still unpublished study, dry needling improved upper limb spasticity as measured by the Modified Modified Ashworth score, and increased passive wrist range of motion compared to controls.
Additional Findings on Dry Needling for Post-Stroke Spasticity
In another Spanish study, patients with post-stroke spasticity received three sessions of dry needling in the shoulder girdle muscles combined with a multimodal rehabilitation program and showed significant improvements in shoulder range of motion, pressure pain thresholds and spasticity in the external rotator muscles, such as the infraspinatus muscle (Mendigutia-Gomez et al. 2016). Calvo and colleagues reported in a case report that dry needling decreased local muscle stiffness assessed by tensiomyography in a patient with chronic post-stroke spasticity (Calvo et al. 2016).
The same research group also published a case report of two post-stroke patients with specific electroencephalographic changes following dry needling. The first subject was treated with dry needling of the pronator teres, medial and lateral gastrocnemius, soleus, and fibularis longus muscles. The second patient received dry needling of the pectoralis major, biceps brachii, brachialis, latissimus dorsi, teres major, pronator teres, flexor digitorum superficialis and profundus, adductor pollicis, medial and lateral gastrocnemius, soleus, semitendinosus, semimembranosus, and the long head of biceps femoris muscles. The researchers documented differences in alpha waves and changes in the cordance of the frontal and prefrontal regions, using quantitative electroencephalographic activity and electroencephalographic cordance (Calvo et al. 2017). One of the authors of this paper, Dr. Pablo Herroro, has presented his work at a conference hosted by Myopain Seminars. Have a look at his lectures (part 1; part 2).
Comparing more traditional Bobath treatments with ultrasound-guided dry needling of the tibialis posterior muscle, researchers found a significantly greater decrease in spasticity in the subjects in the dry needling group along with improved balance, range of motion, and accuracy of maintaining stability (Sanchez-Mila et al. 2018). An Iranian-Spanish study of the effect of dry needling on spasticity, gait, and muscle architecture showed significant improvements 30 minutes after dry needling, but the study did not include a control group and was not blinded.
Dry Needling to Decrease Spasticity From Spinal Cord Injuries
A recent study of 10 sessions of dry needling to decrease spasticity in a patient with a spinal cord injury revealed once again that dry needling resulted in immediate and short-term (10 weeks) improvements of spasticity in the upper and lower limbs as measured by the Modified Ashworth Scale (Cruz-Montecinos et al. 2020). Similarly, a case report of a patient with a brain tumor showed that dry needling improved spasticity, passive and active ankle dorsiflexion, and wrist extension, and several functional tests, such as the Box and Block Test, the Timed Up and Go test (TUG), 10- minute walk, and single-leg stance (Tavakol et al. 2019).
There is now emerging evidence that dry needling can positively influence muscle tone and spasticity in patients with spasticity. Unfortunately, many studies feature small sample sizes, rarely including long-term outcomes and adequate blinding (Braithwaite et al. 2019).
Jan Dommerholt, PT, DPT
Dry Needling Course Series
The Dry Needling 1 course is an excellent starting point for learning the fundamentals of dry needling therapy. With a focus on the safe and effective application of dry needling techniques, you will gain a solid understanding of myofascial trigger points, needling techniques, precautions, and how to apply these techniques in clinical practice.
The Dry Needling 2 course is an intermediate-level course that provides in-depth knowledge and hands-on training for dry needling techniques of the extremities, including the upper and lower body. By completing this course, you will expand upon the skills you acquired in the DN-1 course and better understand the application of dry needling for managing musculoskeletal pain and dysfunction.
The Dry Needling 3 course is the final course in the series and the last step before becoming a Certified Myofascial Trigger Point Therapist – Dry Needling (CMTPT/DN). This course offers an in-depth study of advanced dry needling techniques for hand muscles, several lower extremity and foot muscles, the craniofacial and craniomandibular muscles, and more.
References
Ansari, NN, Naghdi, S, Fakhari, Z, Radinmehr, H & Hasson, S, 2015. Dry needling for the treatment of poststroke muscle spasticity: a prospective case report. NeuroRehabilitation, 36, 61-65.
Braithwaite, FA, Walters, JL, Li, LSK, Moseley, GL, Williams, MT & Mcevoy, MP, 2019. Blinding Strategies in Dry Needling Trials: Systematic Review and Meta-Analysis. Physical Therapy, 99, 1461-1480.
Burridge, JH, Wood, DE, Hermens, HJ, Voerman, GE, Johnson, GR, Van Wijck, F, Platz, T, Gregoric, M, Hitchcock, R & Pandyan, AD, 2005. Theoretical and methodological considerations in the measurement of spasticity. Disability and Rehabilitation, 27, 69-80.
Calvo, S, Navarro, J, Herrero, P, Del Moral, R, De Diego, C & Marijuán, PC, 2017. Electroencephalographic changes after application of dry needling [DNHS[1] Technique] in two patients with chronic stroke. MYOPAIN, online 1-6.
Calvo, S, Quintero, I & Herrero, P, 2016. Effects of dry needling (DNHS technique) on the contractile properties of spastic muscles in a patient with stroke: a case report. International Journal of Rehabilitation Research, 39, 372-376.
Cruz-Montecinos, C, Nunez-Cortes, R, Bruna-Melo, T, Tapia, C, Becerra, P, Pavez, N & Perez-Alenda, S, 2020. Dry needling technique decreases spasticity and improves general functioning in incomplete spinal cord injury: A case report. Journal of Spinal Cord Medicine, 43, 414-418.
Domingo, A, Mayoral, O, Monterde, S & Santafe, MM, 2013. Neuromuscular damage and repair after dry needling in mice. Evid Based Complement Alternat Med, 2013, 260806.
Dommerholt, J & Fernández De Las Peñas, C 2018 Trigger point dry needling; an evidenced and clinical-based approach. Edinburgh, Churchill Livingstone.
Fakhari, Z, Ansari, NN, Naghdi, S, Mansouri, K & Radinmehr, H, 2017. A single group, pretest-posttest clinical trial for the effects of dry needling on wrist flexors spasticity after stroke. NeuroRehabilitation, 40, 325-336.
Fink, M, Rollnik, JD, Bijak, M, Borstadt, C, Dauper, J, Guergueltcheva, V, Dengler, R & Karst, M, 2004. Needle acupuncture in chronic poststroke leg spasticity. Archives of Physical Medicine and Rehabilitation, 85, 667-672.
Gallego, PH & Mayoral, O, 2007. A case study looking at the effectiveness of deep dry needling for the management of hypertonia. J Musculoskeletal Pain, 15, 55-60.
Ghannadi, S, Shariat, A, Ansari, NN, Tavakol, Z, Honarpishe, R, Dommerholt, J, Noormohammadpour, P & Ingle, L, 2020. The Effect of Dry Needling on Lower Limb Dysfunction in Poststroke Survivors. J Stroke Cerebrovasc Dis, 29, 104814.
Lim, SM, Yoo, J, Lee, E, Kim, HJ, Shin, S, Han, G & Ahn, HS, 2015. Acupuncture for spasticity after stroke: a systematic review and meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med, 2015, 870398.
Lim, SM, Yoo, J, Lee, E, Kim, HJ, Shin, S, Han, G & Ahn, HS, 2017. Corrigendum to “Acupuncture for Spasticity after Stroke: A Systematic Review and Meta-Analysis of Randomized Controlled Trials”. Evid Based Complement Alternat Med, 2017, 7324857.
Mendigutia-Gomez, A, Martin-Hernandez, C, Salom-Moreno, J & Fernandez-De-Las-Penas, C, 2016. Effect of Dry Needling on Spasticity, Shoulder Range of Motion, and Pressure Pain Sensitivity in Patients With Stroke: A Crossover Study. Journal of Manipulative and Physiological Therapeutics, 39, 348-358.
Mohammadpour, F, Ali Oghabian, M, Nakhostin Ansari, N, Naghdi, S & Dommerholt, J, 2020. Effects of dry needling on post-stroke brain activity and muscle spasticity of the upper limb: a case report. Acupuncture in medicine : journal of the British Medical Acupuncture Society, 964528420920294.
Mukherjee, M, Mcpeak, LK, Redford, JB, Sun, C & Liu, W, 2007. The effect of electro-acupuncture on spasticity of the wrist joint in chronic stroke survivors. Archives of Physical Medicine and Rehabilitation, 88, 159-166.
Salom-Moreno, J, Sanchez-Mila, Z, Ortega-Santiago, R, Palacios-Cena, M, Truyol-Dominguez, S & Fernandez-De-Las-Penas, C, 2014. Changes in spasticity, widespread pressure pain sensitivity, and baropodometry after the application of dry needling in patients who have had a stroke: a randomized controlled trial. Journal of Manipulative and Physiological Therapeutics, 37, 569-579.
Sanchez-Mila, Z, Salom-Moreno, J & Fernandez-De-Las-Penas, C, 2018. Effects of dry needling on post-stroke spasticity, motor function and stability limits: a randomised clinical trial. Acupuncture in medicine : journal of the British Medical Acupuncture Society, 36, 358-366.
Tavakol, Z, Shariat, A, Ghannadi, S, Noormohammadpour, P, Honarpishe, R, Cleland, JA, Ansari, NN & Moghimi, E, 2019. The effect of dry needling on upper and lower limb spasticity in a patient with a brain tumor. Acupuncture in medicine : journal of the British Medical Acupuncture Society, 37, 133-135.
Wayne, PM, Krebs, DE, Macklin, EA, Schnyer, R, Kaptchuk, TJ, Parker, SW, Scarborough, DM, Mcgibbon, CA, Schaechter, JD, Stein, J & Stason, WB, 2005. Acupuncture for upper-extremity rehabilitation in chronic stroke: a randomized sham-controlled study. Archives of Physical Medicine and Rehabilitation, 86, 2248-2255.
Zhao, JG, Cao, CH, Liu, CZ, Han, BJ, Zhang, J, Li, ZG, Yu, T, Wang, XH, Zhao, H & Xu, ZH, 2009. Effect of acupuncture treatment on spastic states of stroke patients. Journal of the Neurological Sciences, 276, 143-147.